As COVID-19 surged last year, hospitals and medical clinics rushed to secure personal protective equipment (PPE) as supply chains ground to a halt. Factories closed. So did borders. The very pandemic that necessitated more PPE was making it scarce. Supply dwindled as demand soared.
“There were a couple of weeks where we didn’t know if we’d have what we needed,” says Caroline Hennessey, an emergency room nurse in Port Hawkesbury, Nova Scotia.
Hennessey turned to Glia a non-profit organization that makes open source, 3D-printed medical equipment. Glia designs products that can be printed using recycled plastic, so that even clinics in conflict zones can build their own equipment while cut off from access to traditional supply chains.
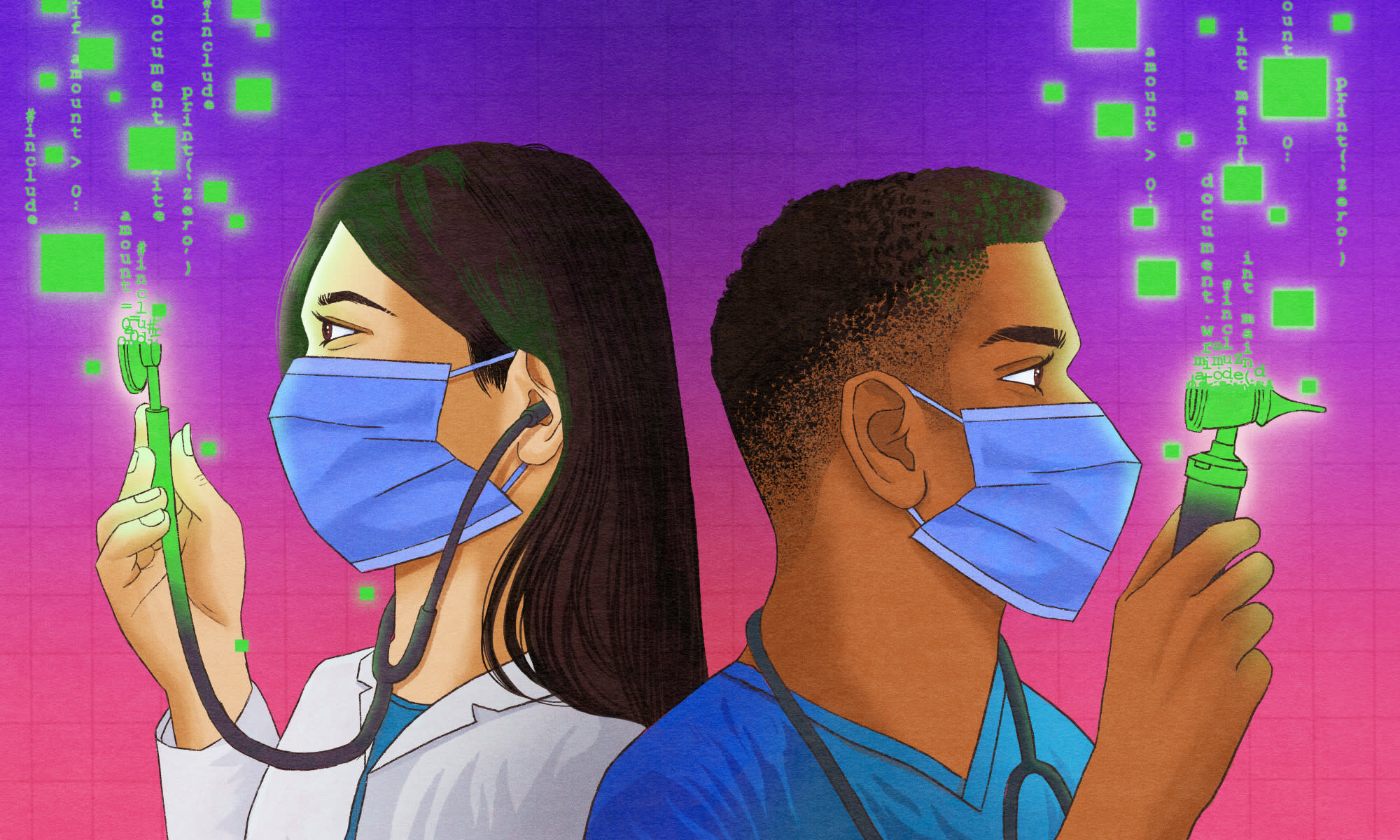
As the world's hospitals and clinics braced for PPE shortages, the Glia team designed an open source face shield and put the organization’s own 3D printers to work. They had seen that smaller hospitals and clinics were suffering, and were able to step-in to help. Hennesy was already familiar with the organization’s 3D-printed stethoscopes, so she ordered enough face shields for all her coworkers. “It felt good having our own equipment,” she says. “It was one less thing to worry about. We could focus more on our patients.”
Glia wasn't alone in 3D printing face shields. Other groups like Prusa released face shield designs, while 3D printing hobbyists around the world pitched in to print. Members of one group, 3D Crowd UK, printed 170,000 face shields from their homes, according to the Wall Street Journal.

Gina Häußge, who maintains the open source 3D printing interface Octoprintsays the project saw big increases in activity during the pandemic. Between early March and early April, print jobs started from Octoprint jumped from 50,000 per day to nearly 100,000. It's difficult to say how many of these were printing PPE, but Häußge says the interest was clear. "I joined several Slack and Discord groups for 3D printing enthusiasts who were helping out during the pandemic," she says. "I couldn't keep up with all the messages—there were so many people offering to help out."
Of course, traditional manufacturers pitched in as well, eventually producing PPE at a scale that 3D printers couldn't match. But groups like Glia helped fill the gap while manufacturers retooled and supply chains rerouted.
The 3D printing community’s response to the PPE shortage points to a new open source and decentralized form of production, one that Glia has been pioneering for years. But the idea extends beyond emergency production. "Our goal is to provide equal medical care to everyone in the world," Glia USA director Jon Philips says.
Dr. Tarek Loubani, a London, Ontario-based ER doctor, started the project that became Glia in 2012 while volunteering at an ER in Gaza. The facility was so severely under-equipped that they only had one stethoscope for 10 doctors. Loubani resorted to putting his ear to patients' chests to listen for a heartbeat. Stethoscopes are a fundamental piece of medical equipment, but top-of-the-line stethoscopes can cost as much as $200 retail. Glia aims to create hardware that is easily accessible and can be manufactured in low-resource settings.
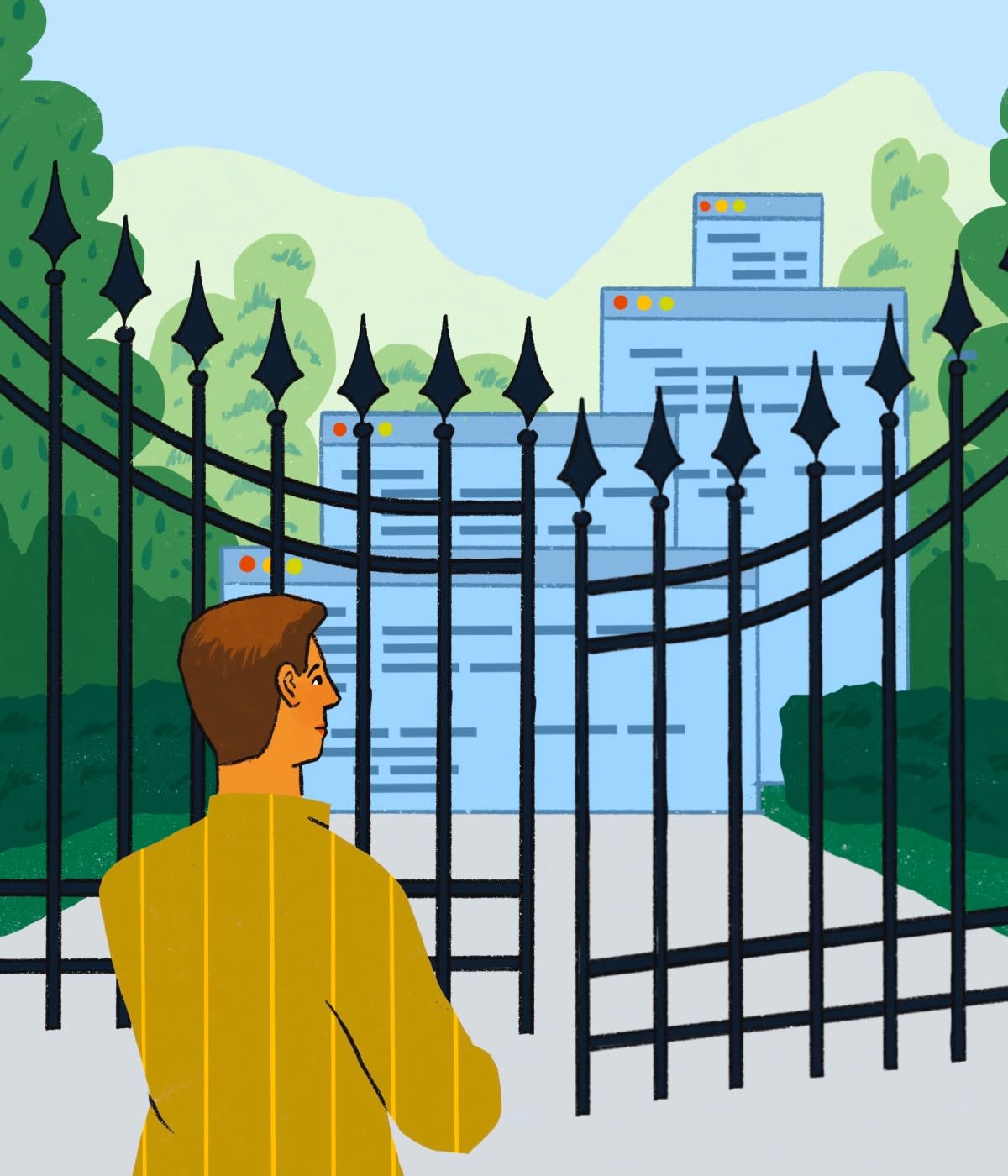
Loubani raised funds to buy stethoscopes and other essentials for Gaza hospitals and clinics, but when the Israeli military blockade kept supplies from reaching hospitals, he realized that he needed to find another way to get equipment into doctors' hands. Inspired by his daughter's toy plastic stethoscope, he hit upon the idea of creating cheap, 3D printable medical equipment.
Loubani built his own 3D printer. Today, there are several low-cost models available off-the-shelf, but Loubani needed a machine that could be built from spare parts—such as the nozzles of old inkjet machines—to ensure that equipment could be made even under a blockade.

For the cost of a single high-end stethoscope, hospitals could buy a machine and, using recycled plastic, manufacture their own medical equipment locally. That would solve both the problem of cost and the dependence on international supply chains. He assembled a group of volunteers from his activist circle with experience in 3D printing and Glia was born.
The team endeavored to produce a stethoscope that could compete with any other on the commercial market. “We didn't want to use the people of Gaza as test subjects,” Loubani explained. “All too often people experiment on the poor. They say ‘we don't know if this works so we'll try it out on you.’ We wanted to bring something to Gaza that we already knew worked.”
After extensive testing and iteration, the Glia team landed on a product they believed could rival a high-end stethoscope but that can be printed in under an hour for less than $3. Hennessey says the Glia stethoscopes live up to the team’s ambitions. “The earbuds might wear and tear a bit more compared to a $200 stethoscope,” Hennessey says. “But in terms of audio quality, it’s just as good.”
In 2018, the Glia stethoscope received regulatory approval in Canada. "Everything we manufacture meets government requirements," Loubani says. Glia soon expanded and developed a 3D-printable tourniquet, another important piece of equipment that was in short supply in Gaza.
Glia opted to release its designs on GitHub under open source licenses. "We already did the work, so we thought no one else should have to go through that process again," Loubani says. Plus it makes it easy for hospitals, clinics, and other groups anywhere in the world to print the designs without having to wait for shipping from Glia's Canadian or US facilities.
Open source communities have built operating systems, programming languages, cloud computing platforms, and artificial intelligence frameworks. Couldn't medical devices be created in the same way? "You can argue about whether the open source model works or not but other models have clearly failed," Loubani says. "The commercial model is all about trade secrets and patents. Our model is about openness and collaboration."
Hanan Abu Qassem, an emergency medical technician in Gaza, was introduced to Glia through a 12-hour training the organization held to teach emergency responders to use the 3D-printed tourniquets. She was so impressed with the tourniquets that she organized more trainings in Gaza and now serves as administrative director for Glia's Gaza office.
Qassem had to rely on that training, and the tourniquets, extensively during the Gaza border protests of 2018 and 2019. "There were many injuries in the field," she says. "The Glia tourniquet saved many lives." She now carries Glia tourniquets not only in her EMT kit but also in the bag she carries every day in case of emergencies like traffic accidents.
The Glia team is now working on an electrocardiogram (a device that traces the heart's electrical activity) and a pulse oximeter (a device for measuring the level of oxygen in your blood). Later they hope to build a dialysis machine. What all three devices have in common is that they’re essential yet expensive equipment based mostly on expired patents. "Knowing a patient's oxygen status is a fundamental aspect of surgery," Loubani says. "But across the world, there are operating rooms that lack pulse oximeters."
In addition to open sourcing their work, Glia is drawing on existing work from the open source community. Glia’s electrocardiogram is based on electrocardiogram designs open sourced by Hungarian engineers Peter Iszaand Csordás Róbert. "It must have saved us years of design work," Loubani says. "We contacted them, and they were so happy to see their baby out in the world."
Glia is hoping to find more collaborators to bring these projects to fruition—the pulse oximeter has proven particularly challenging to perfect. “The whole purpose of open source is to bring together people with different strengths,” says Kate Kazlovich, a clinical engineering PhD candidate at the University of Toronto who has been helping design and validate Glia devices. “Not every doctor has access to the skills and equipment an engineer does, and not every engineer has the knowledge and background of a medical doctor.”
Open source has already worked wonders in the software world. We’re only just beginning to see what kinds of innovation this collaborative model can unleash in the hardware world.